When treating patients, healthcare providers must document each session as accurately as possible. With accurate patient documentation, the team can keep track of the treatments provided to the patient. It also allows them to chart the appropriate steps to ensure the patient recovers on time. In fact, a study by JAMA Internal Medicine found that physicians spend an average of 1.84 hours per day conducting documentation duties outside their working hours because of how important they are to their work.
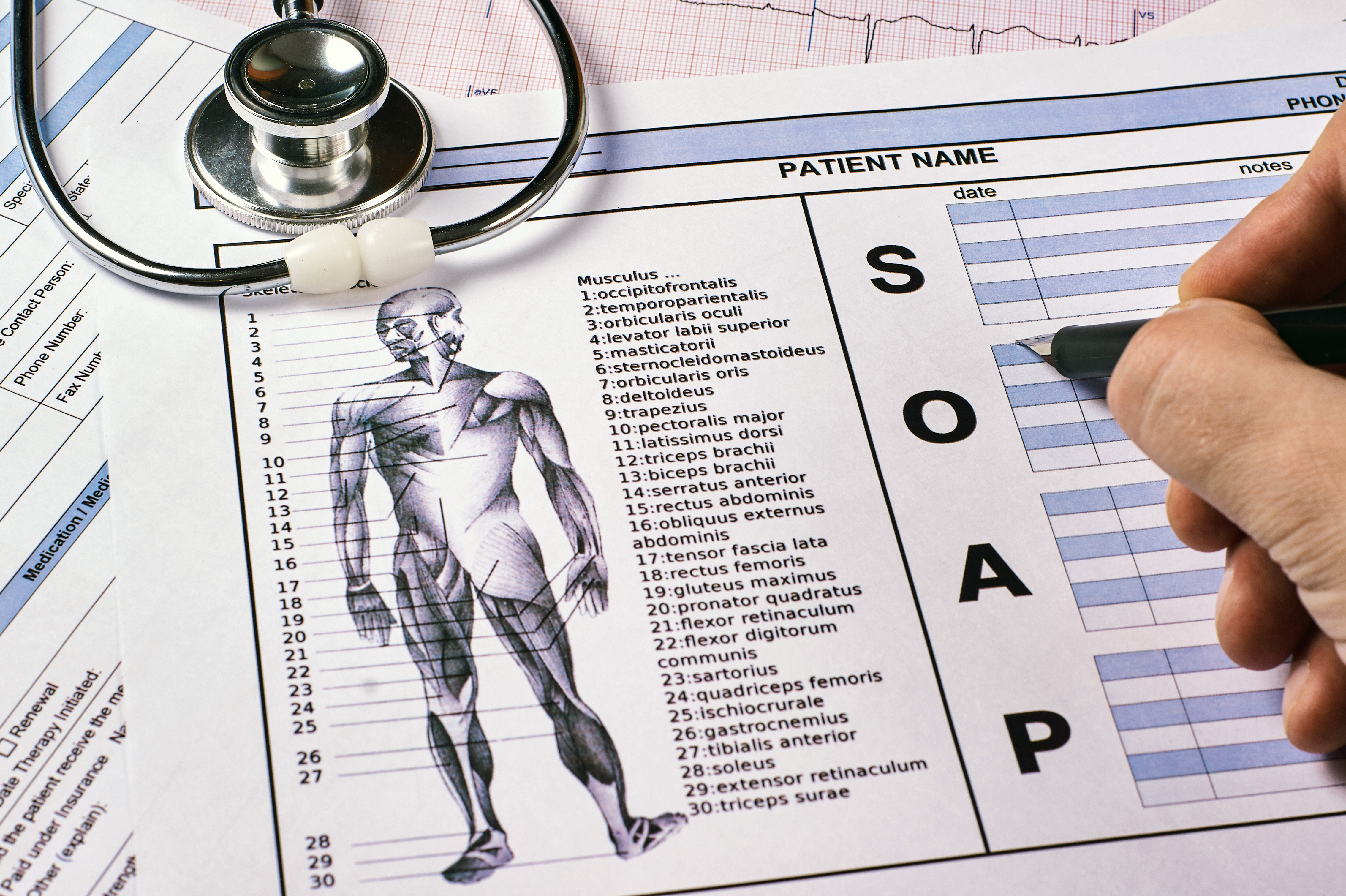
Healthcare professionals can use various types of notes to record patient sessions properly. Often, the type of note used depends on the patient's current problem. In physical therapy, the most common type is SOAP Notes.
But what are SOAP notes, and how do they help physical therapists? Read on to learn everything you need to know about this type of documentation.
The History of SOAP Notes
The history of SOAP notes can be traced back to 1971, when Yale University professor Dr. Lawrence Weed noticed the lack of a standardized process for clinical documentation. This led to the development of the precursor to SOAP notes: the Problem-Oriented Medical Record (POMR).
The primary purpose of the POMR is to provide healthcare providers with structure when documenting patient sessions. Additionally, it helps remind them of specific tasks. The SOAP note eventually emerged as a branch of the POMR, with SOAP only associated with one of the problems identified by the provider. This meant that SOAP notes were only one part of the patient documentation process.
However, the POMR gradually fell by the wayside and wasn’t widely adopted by the healthcare industry, which favored SOAP notes more for documenting patient sessions.
SOAP Notes: What Do They Mean?
Are you still wondering what are SOAP notes in physical therapy? In a nutshell, SOAP stands for Subjective, Objective, Assessment, and Plan. To fully comprehend the role of SOAP notes in physical therapy, it’s best to dive further into each component of the SOAP note.
Subjective
The first part of the SOAP note is the Subjective section. Here, physical therapists take down the information that they collect directly from the patient. Often, this includes the patient’s main complaint, history with their current problem, and overall medical and surgical history (which also includes their family’s medical history). The medication that the patient currently takes, their doses, and the administration frequency may also be included in this section.
Objective
After the Subjective portion of the SOAP note comes the Objective section. In this part of the physical therapy documentation, vital signs and other measurable terms in the patient’s treatment will be written. That way, assessments can be conducted more easily, which can help PTs analyze patient progression. This, in turn, lets them determine what helps or hinders the patient’s treatment.
Apart from the measurable terms in treatment, any changes in the patient’s status are noted in the Objective section of the SOAP note. Communication with colleagues and the patient’s family is also included here.
Assessment
The Assessment section of the documentation is said to be the most important part of the note. This is because the physical therapist’s professional opinion is written here after taking the Subjective and Objective findings into account. When writing the Assessment section, the PT must explain the reasoning behind the treatment interventions they’ve made.
In addition, this section of the PT documentation usually indicates the patient’s progress in the treatment and any factors that could affect its effectiveness.
Plan
The final part of SOAP notes for physical therapy is the Plan section. Here, the treatment plan for the patient is outlined. Other details such as treatment frequency, specific interventions (and any changes to it), progression, and even the equipment that will be used are recorded in this section. Additionally, referrals to other healthcare providers and recommendations regarding the patient’s follow-up care are included here.
The Goals Section: What Is It and Where Does It Go?
Physical therapy SOAP notes have another component as vital as the rest. This component is known as the Goals, which refers to the ideal outcomes of the patient’s treatment. Often, it indicates the physical therapy exercises that will be conducted as well as the purpose of said exercise.
The Goals section is usually placed before the Subjective section or after the Plan section of the note. Some PTs mix it with the Plan section if it better suits the clinical team’s comprehension of the note.
Using the SOAP notes format can greatly help a physical therapist when recording patient sessions. It also helps the entire team remain updated on the patient’s status and treatments and improves communication between physical therapists. As such, SOAP notes should remain accurate as much as possible. If you’re looking for an advanced solution to help you along the way, look no further than ScribePT.
ScribePT is an AI tool tailored to assist providers in documentation for physical therapy. It boasts advanced features such as one-click EMR transfer, quick edits, and instant transcripts thanks to real-time recording, allowing PTs to save time and reclaim up to 40 hours of their time every month. Request a demo right now to see ScribePT’s time-saving capabilities for yourself!