Highlights
Interoperability allows different healthcare systems to share patient data securely: which reduces medical errors and improves safety.
Modern data standards like HL7 and FHIR enable physical therapy clinics to coordinate care seamlessly with hospitals and primary physicians.
Automated data exchange reduces the administrative load on clinicians: helping to mitigate the 18% turnover rate currently seen in technical healthcare roles.
Nowadays, technology permeates many aspects of our lives. Socializing, communications, businesses; almost everything relies on technology to run smoothly. Physical therapy and healthcare, in general, are no exception. In fact, healthcare today runs on a system known as “interoperability.”
But what is it, and why is interoperability important in healthcare? Here’s everything you need to know.
What Is Interoperability in Healthcare?
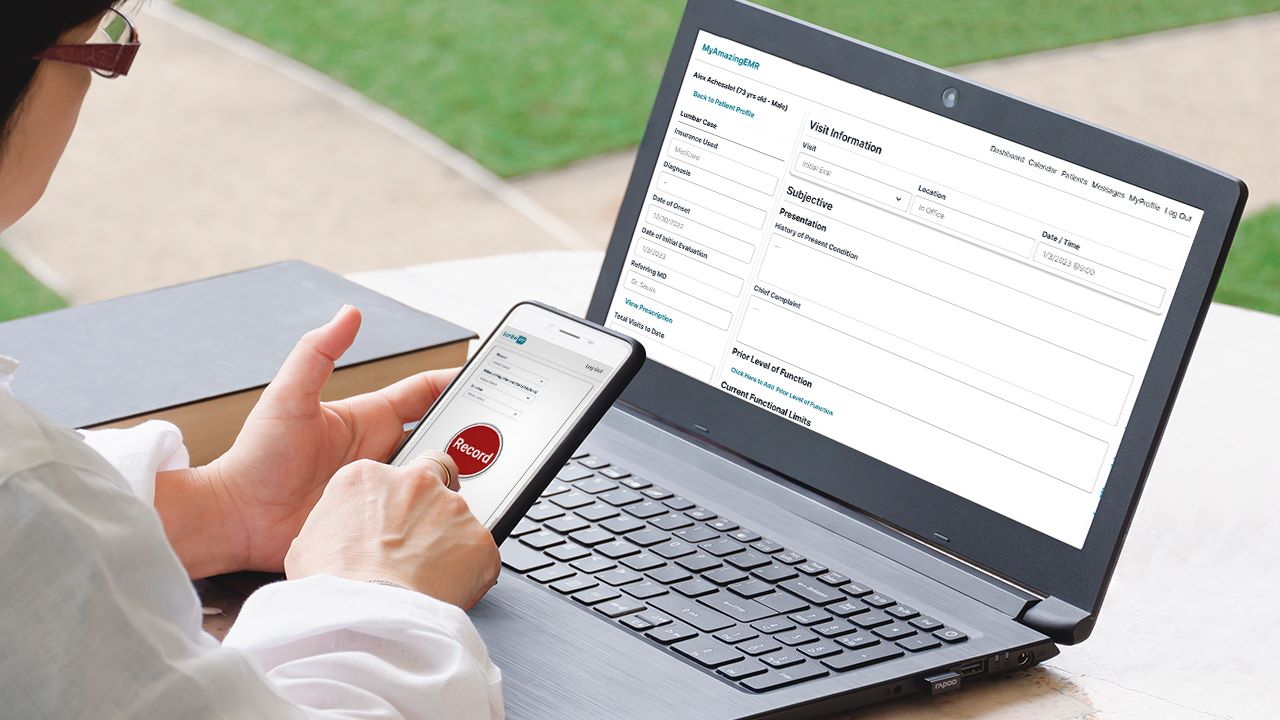
Interoperability is the ability of different information systems and software applications to communicate and exchange data accurately. In a clinical setting: this means your Electronic Medical Record (EMR) system can send and receive information from other providers without manual entry. It relies on shared standards to ensure that data remains consistent across different platforms.
Why Is Interoperability Essential for Physical Therapy?
Physical therapy often functions as part of a broader care plan involving surgeons: primary care doctors: and specialists. Without interoperability: patient information remains trapped in silos. Effective data exchange is vital for maintaining HIPAA compliance and ensuring care continuity.
1. How Does Interoperability Increase Patient Safety?
Interoperability ensures that every provider has access to a complete patient history. This includes current medications: previous surgeries: and imaging results. When systems share data: clinicians avoid the common problems with medical documentation that lead to treatment errors. Access to real-time data prevents clinicians from prescribing exercises or modalities that might conflict with a patient's medical status.
2. Can Interoperability Improve Clinic Efficiency?
Manual data entry is a primary cause of clinical burnout. Recent data shows that healthcare practitioners face high administrative stress: which contributes to rising turnover rates. Interoperability automates the transfer of referral information and diagnostic reports. This reduces the time staff spend on faxing or calling other offices. By using interoperable AI solutions: clinics can focus on patient volume rather than paperwork.
3. How Does It Facilitate Better Care Coordination?
Physical therapists often need to report progress back to referring physicians. Interoperable systems allow for the instant sharing of physical therapy SOAP notes. When the primary doctor sees the functional gains a patient makes in therapy: they can adjust the overall plan of care. This collaboration is a hallmark of effective interdisciplinary communication.
The Technical Standards Powering Data Exchange
For interoperability to work: software must follow specific protocols. Modern systems use Health Level Seven (HL7) and Fast Healthcare Interoperability Resources (FHIR). These frameworks allow your EMR ecosystem to talk to hospital databases. This technical alignment is what enables a One-Click Paste-to-EMR workflow: ensuring that AI clinical documentation moves where it is needed most.
Strategic Advantages for Rehab Practices
Clinics that adopt interoperable technology gain a competitive edge. They attract more referrals because they make it easy for other doctors to work with them. They also experience higher patient satisfaction. Patients do not have to repeat their medical history at every appointment because the data is already in the system. Investing in interoperability is an investment in the long-term growth of the practice.